Personalised Pathology – A Vision for the Future
Imagining the future we want is the first step to realizing it. Personalised medicine can help to improve health outcomes for cancer patients – and molecular pathology is a key enabler. So what does the future of molecular pathology look like?
Dr. Clarke

Imagination can be a powerful tool for achieving progress. Building a vision of a positive future can spur us into action and help us plan how to achieve our goals. In the Future of Pathology Report, I talk a lot about the huge potential for molecular pathology and the many benefits it can bring to patients, to overstretched healthcare professionals working to tackle the rising number of cancer cases,1,2 and to health services that cannot run without cost and resource efficiencies. In this blog post, I want to imagine what the future might look like for a cancer patient if we’re able to achieve the progress we would like. This is a future where widespread, appropriate use of molecular pathology is the norm, but also where improvements to the other areas we discuss in the Future of Pathology Report have been implemented. Namely, improvements relating to education, technology, and the perception and profile of pathologists.
So imagine this with me. Jim* is a middle-aged man who has had a persistent cough which has been a distraction at work and disturbing his sleep. He lives alone and doesn’t want to bother his doctor, but it has been steadily getting worse. Finally, he decides to see his GP and is referred for a chest X-ray. The result shows evidence of a mass in his left lung. He undergoes a biopsy of the mass which is then sent to the pathology team.
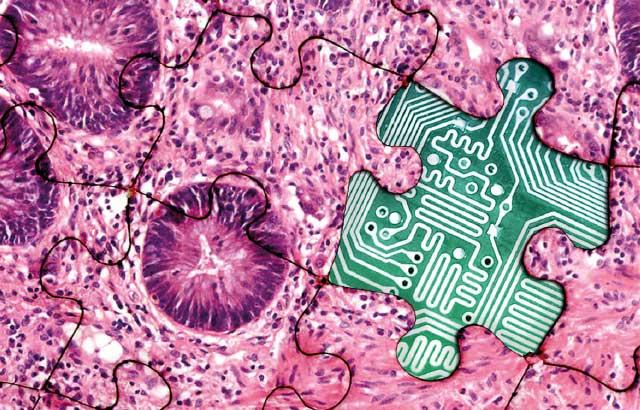
In the lab, a well-resourced and equipped team of pathologists immediately diagnoses the problem. Jim has a tumour in his left lung. Firstly, the team looks at the microscopic appearance of the tumour to give them an idea of the type of cancer they are dealing with. They then go a step further and remove the genetic material (DNA and RNA) from the cells and use it and other material of the tumour to perform a combination of advanced molecular techniques, supplemented by the latest tools of artificial intelligence, to give a much more detailed picture of the type of tumour. By integrating all the information from both the microscopic examination and the molecular testing, the team are able to provide an accurate diagnosis and state confidently not only what type of tumour it is but also what subtype, and if there are targetable options for treatment. Given Jim’s age and some of the other health issues he might have, there are a variety of treatment choices available to him.
The pathology team contacts Jim’s oncology team using a secure, digital platform to share their findings. Without delay, the oncologists immediately add the notes to the next multidisciplinary team meeting, which pathologists attend that afternoon. There is trust and understanding between the pathology and oncology team. Hospital administrators also recognize the expertise of the pathology team and have increasingly encouraged pathologists to join consultations with patients, helping them to understand more about their cancer. Some patients find this to be a helpful way of coping with their diagnosis.3
Following an initial consultation to tell Jim the diagnosis, a pathologist and oncologist talk Jim through his diagnosis and treatment options as a combined team. Jim opts to have the tumour removed by an operation. The tumour is sent to the pathology lab and the same tests are performed, confirming the diagnosis. He then begins his treatment, supervised by his oncologist.
A few months later, a body scan shows that some of Jim’s tumour has grown back. Jim undergoes a repeat biopsy and another set of tests are performed by the pathology team. The tests let them see if and how the tumour has changed or evolved. The oncologists change Jim’s treatments in response to the test results. Throughout his treatment journey, the pathology team keeps in touch with Jim and helps him see the progress he is making with his cancer. Jim celebrates that he is ‘all-clear’ of cancer in a follow-up scan just a few weeks later; the new test results provided valuable information to enable the successful treatment of the recurrence of Jim’s cancer.
I hope you enjoyed the vision that I created. The point I’m trying to make is that, if we take the right course, these changes are just around the corner for most pathology services and are within our grasp even today. The first step to bringing these changes about is to talk about the issues we are facing, to have the conversations we need to have with our colleagues across the cancer care continuum. On behalf of all the Future of Pathology panel, we hope our Report will start the conversation and make this positive future vision a reality for every patient.
*Persona is a fictional representation
Follow #TheFutureOfPathology on Twitter, Facebook or LinkedIn.
발표자 소개

Histopathology Trainee and Clinical Fellow at the Institute of Cancer Research (London, UK)
참조 문헌
1. Maddams J, Utley M, Møller H. Projections of cancer prevalence in the United Kingdom, 2010–2040, Br J Cancer 2012;107:1195–1202.
2. International Agency for Research on Cancer. World Cancer Report 2014. Lyon, France, 2014. https://www.who.int/cancer/publications/WRC_2014/en/ Accessed 9 June 2020.
3. Booth A, Katz MS, Misialek MJ, et al. ‘‘Please help me see the dragon I am slaying’’. Arch Pathol Lab Med 2019;143:852–858.
Related Content
라이카 바이오시스템즈 Knowledge Pathway 콘텐츠는 에서 이용할 수 있는 라이카 바이오시스템즈 웹사이트 이용 약관의 적용을 받습니다. 법적고지. 라이카 바이오시스템즈 웨비나, 교육 프레젠테이션 및 관련 자료는 특별 주제 관련 일반 정보를 제공하지만 의료, 규정 또는 법률 상담으로 제공되지 않으며 해석되어서는 안 됩니다. 관점과 의견은 발표자/저자의 개인 관점과 의견이며 라이카 바이오시스템즈, 그 직원 또는 대행사의 관점이나 의견을 나타내거나 반영하지 않습니다. 제3자 자원 또는 콘텐츠에 대한 액세스를 제공하는 콘텐츠에 포함된 모든 링크는 오직 편의를 위해 제공됩니다.
모든 제품 사용에 다양한 제품 및 장치의 제품 정보 가이드, 부속 문서 및 작동 설명서를 참조해야 합니다.
Copyright © 2025 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.