Personalised Pathology – A Vision for the Future
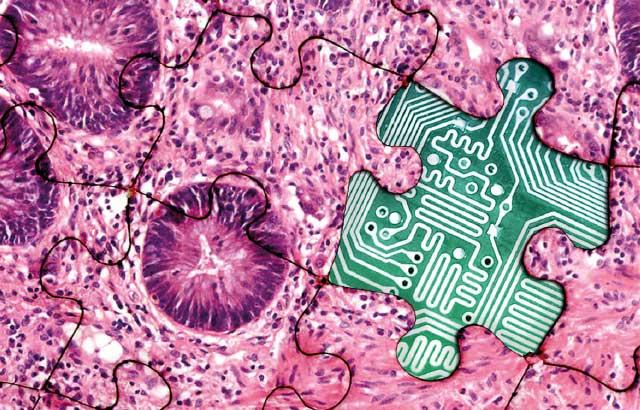
Imagining the future we want is the first step to realizing it. Personalised medicine can help to improve health outcomes for cancer patients – and molecular pathology is a key enabler. So what does the future of molecular pathology look like?
Dr. Clarke

Imagination can be a powerful tool for achieving progress. Building a vision of a positive future can spur us into action and help us plan how to achieve our goals. In the Future of Pathology Report, I talk a lot about the huge potential for molecular pathology and the many benefits it can bring to patients, to overstretched healthcare professionals working to tackle the rising number of cancer cases,1,2 and to health services that cannot run without cost and resource efficiencies. In this blog post, I want to imagine what the future might look like for a cancer patient if we’re able to achieve the progress we would like. This is a future where widespread, appropriate use of molecular pathology is the norm, but also where improvements to the other areas we discuss in the Future of Pathology Report have been implemented. Namely, improvements relating to education, technology, and the perception and profile of pathologists.
So imagine this with me. Jim* is a middle-aged man who has had a persistent cough which has been a distraction at work and disturbing his sleep. He lives alone and doesn’t want to bother his doctor, but it has been steadily getting worse. Finally, he decides to see his GP and is referred for a chest X-ray. The result shows evidence of a mass in his left lung. He undergoes a biopsy of the mass which is then sent to the pathology team.
In the lab, a well-resourced and equipped team of pathologists immediately diagnoses the problem. Jim has a tumour in his left lung. Firstly, the team looks at the microscopic appearance of the tumour to give them an idea of the type of cancer they are dealing with. They then go a step further and remove the genetic material (DNA and RNA) from the cells and use it and other material of the tumour to perform a combination of advanced molecular techniques, supplemented by the latest tools of artificial intelligence, to give a much more detailed picture of the type of tumour. By integrating all the information from both the microscopic examination and the molecular testing, the team are able to provide an accurate diagnosis and state confidently not only what type of tumour it is but also what subtype, and if there are targetable options for treatment. Given Jim’s age and some of the other health issues he might have, there are a variety of treatment choices available to him.
The pathology team contacts Jim’s oncology team using a secure, digital platform to share their findings. Without delay, the oncologists immediately add the notes to the next multidisciplinary team meeting, which pathologists attend that afternoon. There is trust and understanding between the pathology and oncology team. Hospital administrators also recognize the expertise of the pathology team and have increasingly encouraged pathologists to join consultations with patients, helping them to understand more about their cancer. Some patients find this to be a helpful way of coping with their diagnosis.3
Following an initial consultation to tell Jim the diagnosis, a pathologist and oncologist talk Jim through his diagnosis and treatment options as a combined team. Jim opts to have the tumour removed by an operation. The tumour is sent to the pathology lab and the same tests are performed, confirming the diagnosis. He then begins his treatment, supervised by his oncologist.
A few months later, a body scan shows that some of Jim’s tumour has grown back. Jim undergoes a repeat biopsy and another set of tests are performed by the pathology team. The tests let them see if and how the tumour has changed or evolved. The oncologists change Jim’s treatments in response to the test results. Throughout his treatment journey, the pathology team keeps in touch with Jim and helps him see the progress he is making with his cancer. Jim celebrates that he is ‘all-clear’ of cancer in a follow-up scan just a few weeks later; the new test results provided valuable information to enable the successful treatment of the recurrence of Jim’s cancer.
I hope you enjoyed the vision that I created. The point I’m trying to make is that, if we take the right course, these changes are just around the corner for most pathology services and are within our grasp even today. The first step to bringing these changes about is to talk about the issues we are facing, to have the conversations we need to have with our colleagues across the cancer care continuum. On behalf of all the Future of Pathology panel, we hope our Report will start the conversation and make this positive future vision a reality for every patient.
*Persona is a fictional representation
Follow #TheFutureOfPathology on Twitter, Facebook or LinkedIn.
About the presenter

Histopathology Trainee and Clinical Fellow at the Institute of Cancer Research (London, UK)
Referencias
1. Maddams J, Utley M, Møller H. Projections of cancer prevalence in the United Kingdom, 2010–2040, Br J Cancer 2012;107:1195–1202.
2. International Agency for Research on Cancer. World Cancer Report 2014. Lyon, France, 2014. https://www.who.int/cancer/publications/WRC_2014/en/ Accessed 9 June 2020.
3. Booth A, Katz MS, Misialek MJ, et al. ‘‘Please help me see the dragon I am slaying’’. Arch Pathol Lab Med 2019;143:852–858.
Related Content
El contenido de Leica Biosystems Knowledge Pathway está sujeto a las condiciones de uso del sitio web de Leica Biosystems, disponibles en: Aviso legal.. El contenido, incluidos los webinars o seminarios web, los recursos de formación y los materiales relacionados, está destinado a proporcionar información general sobre temas concretos de interés para los profesionales de la salud y no está destinado a ser, ni debe interpretarse como asesoramiento médico, normativo o jurídico. Los puntos de vista y opiniones expresados en cualquier contenido de terceros reflejan los puntos de vista y opiniones personales de los ponentes/autores y no representan ni reflejan necesariamente los puntos de vista ni opiniones de Leica Biosystems, sus empleados o sus agentes. Cualquier enlace incluido en el contenido que proporcione acceso a recursos o contenido de terceros se proporciona únicamente por comodidad.
Para el uso de cualquier producto, debe consultarse la documentación correspondiente del producto, incluidas las guías de información, los prospectos y los manuales de funcionamiento.
Copyright © 2025 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.