
Fixation and Fixatives (2) – Factors Influencing Chemical Fixation, Formaldehyde and Glutaraldehyde

This second part of the Fixation and Fixatives series covers the factors that influence the rate and effectiveness of tissue fixation as well as looking at two common fixatives: formaldehyde (histology) and glutaraldehyde (ultrastructural electron microscopy studies).
Factors influencing chemical fixation
There are a number of factors that will influence the rate and effectiveness of tissue fixation.
Temperature: Increasing the temperature of fixation will increase the rate of diffusion of the fixative into the tissue and speed up the rate of chemical reaction between the fixative and tissue elements. It can also potentially increase the rate of tissue degeneration in unfixed areas of the specimen. For light microscopy initial fixation is usually carried out at room temperature and this may be followed by further fixation at temperatures up to 45°C during tissue processing. This is really a compromise that appears to be widely accepted to produce good quality morphological preservation. Microwave fixation may involve the use of higher temperatures, up to 65°C, but for relatively short periods. See Part 5 for further discussion.
Time: The optimal time for fixation will vary between fixatives. For fixation to occur the fixative has to penetrate, by diffusion, to the center of the specimen and then sufficient time has to be allowed for the reactions of fixation to occur. Both diffusion time and reaction time depend on the particular reagent used, and the optimum time will vary from fixative to fixative. In busy diagnostic laboratories there is considerable pressure to reduce turnaround time and this can result in incompletely-fixed tissues being processed. This can lead to poor quality sections showing tissue distortion and poor quality staining because poorly fixed tissue does not process well. Remember that if incompletely-fixed tissue is taken from formalin and placed in ethanol during processing, ethanol will continue to fix the tissue and the morphological picture at the center of the specimen will be that of ethanol fixation.
Penetration rate: The penetration rate of a fixing agent depends on its diffusion characteristics and varies from agent to agent. As devised by Medawar it can be expressed as d = K√t, where d is the depth of penetration, K is the coefficient of diffusion (specific for each fixative), and t is the time. 1 In practical terms this means that the coefficient of diffusion (K) is the distance in millimeters that the fixative has diffused into the tissue in one hour. For 10% formalin K = 0.78. This means that your formalin fixative should not be expected to penetrate more than say 1 mm in an hour, and it will take approximately 25 hours to penetrate to the center of a 10 mm thick specimen , i.e. 5 mm ( = 5² hours).
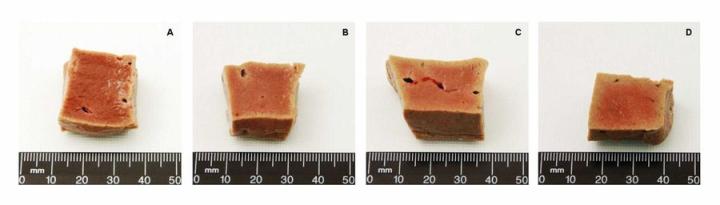
Specimen dimensions: The preceding approximations emphasise the importance of specimen dimensions when fixing tissue. A specimen should not be more than 4 mm thick. Ideally a 3 mm thick slice should provide excellent fixation and processing. It is useful to remember that the specimen cavity in a standard processing cassette is 5 mm deep.
Volume ratio: It is important to have an excess volume of fixative in relation to the total volume of tissue because with additive fixatives the effective concentration of reagent is depleted as fixation proceeds and in a small total volume this could have an effect on fixation quality. A fixative to tissue ratio of 20:1 is considered the lowest acceptable ratio, but I would advocate a target ratio of 50:1.
pH and buffers: At the light microscope level the pH of a fixative does not appear to affect the quality of preservation greatly as a number of formulations have quite a low pH, such as those containing acetic or picric acids. However, pH can be important for other reasons as in the case of formaldehyde solutions, where breakdown of formaldehyde to form formic acid produces an acidic solution which in turn reacts with hemoglobin to produces an artefact pigment (acid formaldehyde hematin). The most popular formaldehyde solution in use today is therefore buffered to pH 6.8 – 7.2 for this reason. For electron microscopy pH is more important and should match physiological pH. 2
Osmolality: The osmotic effects exerted by the fixative are again more important at the ultrastructural level than at the level of the light microscope because it is the phospholipid membranes that are easily damaged by excessively hypotonic or hypertonic solutions, but osmolality does have some relevance in routine histopathology. Generally it is the osmolality of the vehicle (buffer) that is most important and in some formulations this is adjusted to resemble that of tissue fluid (eg. formalin in isotonic saline). Before fixation occurs cells can certainly be damaged by non-isotonic fluids such as water and if specimens cannot be immediately fixed they can be kept moist with gauze soaked in isotonic saline for a short time. It is not a good idea to hold tissue immersed in saline for extended periods.
Fixing agents
There are a number of reagents that can be used to fix tissues. Formaldehyde, by far the most popular agent used for histopathology and glutaraldehyde, widely used for ultrastructural studies requiring electron microscopy, are described here. Other reagents are discussed in Part 3.
Formaldehyde: Formaldehyde (CH2O) is the only gaseous aldehyde and is dissolved in water to saturation at 37% – 40% w/v. This solution is generally referred to as “formalin” or “concentrated formaldehyde solution”. For fixation, one part formalin is usually diluted with nine parts of water or buffer. This produces a 10% formalin solution which contains about 4% formaldehyde w/v, an optimal concentration for fixation. In concentrated solutions formaldehyde exists as its monohydrate methylene glycol and as low molecular weight polymeric hydrates. In its diluted form the monohydrate predominates. Paraformaldehyde, a highly polymerised form of formaldehyde may be deposited as a white precipitate in concentrated formaldehyde solutions. To prevent this, small quantities of methanol (up to 15%) are commonly added to proprietary solutions. Paraformaldehyde can be purchased as a dry powder and used to make up highly pure solutions of formaldehyde such as those required for electron microscopy. 2, 3
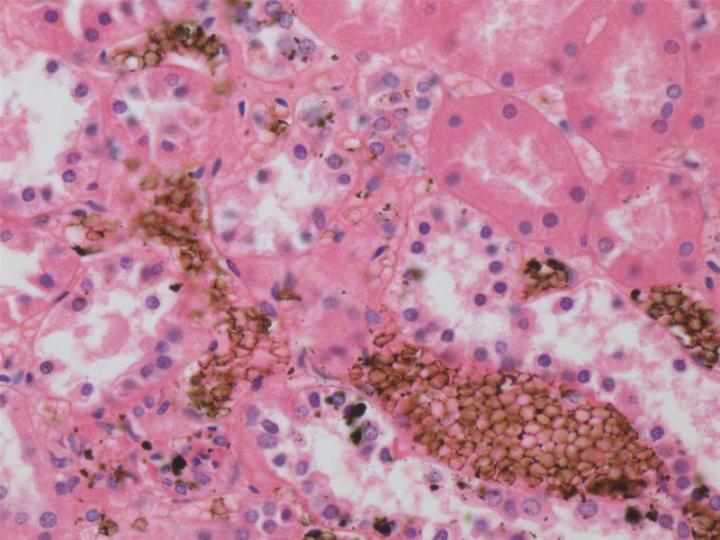
Unbuffered formalin will slowly oxidize to formic acid resulting in a fall in pH. Under these conditions the formic acid will react with hemoglobin forming acid formaldehyde hematin, a brown-black granular artefact pigment which is deposited in blood-rich tissues. This pigment is a nuisance as it can be confused with micro organisms or other pathological pigments. 4 Although the pigment can be removed from sections with saturated aqueous picric acid before staining, it is preferable to avoid its formation in the first place. For this reason and because formaldehyde reacts most effectively at about a neutral pH, 10% formalin solutions are usually buffered to pH 6.8 – 7.2.
Formaldehyde reacts with the side-chains of proteins to form reactive hydroxy-methyl groups. It can penetrate nuclear proteins and nucleic acids stabilizing the nucleic acid-protein shell and modifying the nucleotides by reacting with free amino groups. Formaldehyde can react with some groups in unsaturated lipids particularly if calcium ions are present, but tends to be unreactive with carbohydrates. 5 Formaldehyde can react with groups on lysine, arginine, cysteine, tyrosine, threonine, serine and glutamine forming reactive complexes which may combine with each other forming methylene bridges (cross-links) or with hydrogen groups. 5 It is widely accepted that washing tissues after formalin fixation can reverse some of these reactions but important cross-links remain. 6 It is the ability of formaldehyde to preserve the peptides of cellular proteins which have made it so useful as a general purpose fixative.
There are well known hazards associated with the use of formaldehyde as a fixative through skin or eye contact or via the respiratory tract. It is irritant, corrosive and may cause allergic sensitization. From 1981 formaldehyde was listed as “reasonably anticipated to be a human carcinogen” and in 2011 the listing has been upgraded to “known to be a human carcinogen”.7, 8 Studies have shown that formaldehyde causes nasopharangeal cancer, sinonasal cancer and myeloid leukaemia. For these reasons in most countries there are strict guidelines in place to limit the exposure of workers to formaldehyde in the workplace. For example in the USA the OSHA permissible exposure limit (PEL) is 0.75 ppm (8 hour TWA) and a short-term exposure limit (STEL) of 2 ppm (15 min exposure) and these recommendations are supported by a regular monitoring program. In a well-equipped laboratory with modern fume-extraction equipment these target levels should not be exceeded.9, 10
Despite the risks in using formaldehyde most morphologies have built up their knowledge of normal and diseased tissues by looking at formalin fixed specimens. As we are now aware of the toxic hazards of this reagent many laboratories have sought and are continuing to seek a safer alternative. However, alternatives to formalin are generally judged on their ability to produce a morphological picture similar to, if not better than that produced by formalin and allow a full range of staining methods including molecular methods and be just as cheap. Most labs continue to use formalin because they cannot find a completely satisfactory replacement, so it is important that staff are aware of the hazards involved. Some alternatives to formaldehyde are discussed in Part 3.
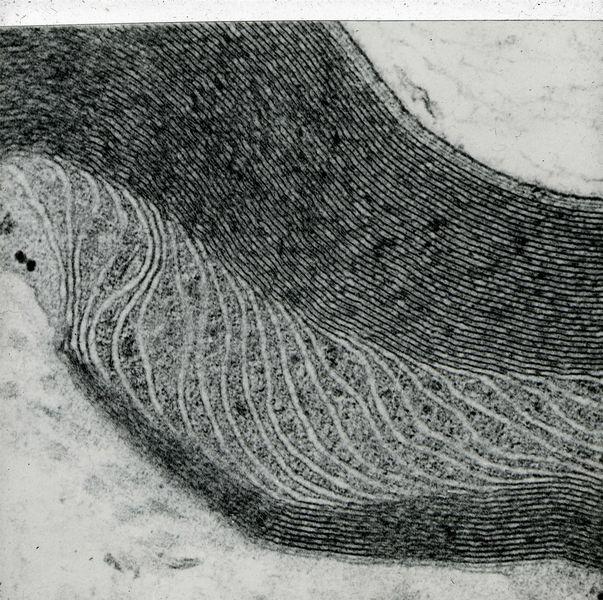
Glutaraldehyde: Glutaraldehyde or glutaric dialdehyde (CHO(CH2)3CHO) Is regarded as a bifunctional aldehyde, possessing aldehyde groups at either end of the molecule which have the potential to react with the same chemical groups as formaldehyde. They will form addition compounds and methylene bridges, but also a single glutaraldehyde molecule may form direct-cross links if the steric arrangement of adjacent peptides allow it. The amino groups of lysine are particularly important in this respect. Tissue fixed in glutaraldehyde will be more extensively cross-linked than tissue fixed in formalin and will also possess some unreacted aldehyde groups that, unless chemically blocked, can cause background staining in methods such as PAS. The extensive cross-linking adversely affects immunohistochemical staining but does provide excellent ultrastructural preservation which explains its extensive use as a primary fixative for electron microscopy. Cross-linking reactions of glutaraldehyde are largely irreversible. Glutaraldehyde penetrates very slowly and it is recommended that tissue be less than 1mm in thickness in at least one dimension. 5, 11
Glutaraldehyde will slowly decompose to form glutaric acid and will also polymerise to form cyclic and oligomeric compounds. Glutaraldehyde is therefore best obtained in sealed ampoules in a convenient form “stabilized for electron microscopy” and this can be added to a suitable buffer at pH 7.2 – 7.4 (usually cacodylate, phosphate or maleate) to produce a 3% glutaraldehyde concentration for use. For electron microscopy glutaraldehyde primary fixation is commonly followed by secondary fixation in osmium tetroxide. Glutaraldehyde is not normally used for routine histopathology. 11

About the presenter

Geoffrey Rolls is a Histology Consultant with decades of experience in the field. He is a former Senior Lecturer in histopathology in the Department of Laboratory Medicine, RMIT University in Melbourne, Australia.
References
- Medawar PB. The rate of penetration of fixatives. J Royal Micros Soc 1941;61;46-57.
- Carson FL. Histotechnology. 2nd ed. Chicago: ASCP Press, 1997.
- Leong AS-Y. Fixation and fixatives. In Woods AE and Ellis RC eds. Laboratory histopathology. New York: Churchill Livingstone, 1994;4.1-1 - 4.1-26.
- Rolls GO, Farmer NJ, Hall JB. Artifacts in histological and cytological preparations. In Woods A and Ellis R eds. Laboratory histopathology. New York: Churchill Livingstone, 1994;5.3-1 - 5.3-29.
- Eltoum I, Fredenburgh J, Myers RB, Grizzle WE. Introduction to the theory and practice of fixation of tissues. J Histotechnol 2001;24;173 -190.
- Eltoum I, Fredenburgh J, Grizzle WE. . Advanced concepts in fixation: 1. Effects of fixation on immunohistochemistry, reversibility of fixation and recovery of proteins, nucleic acids, and other molecules from fixed and processed tissues. 2. Developmental methods of fixation. J Histotechnol 2001;24;201-210.
- NTP. Report on carcinogens, Twelfth Edition. National Toxicology Program, USA Department of Health and Human Services, 2011; http://ntp.niehs.nih.gov/ntp/roc/twelfth/roc12.pdf November 7, 2011
- NTP. Addendum to the 12th Report on Carcinogens. USA Department of Health and Human Services, National Toxicology Program, 2011; http://ntp.niehs.nih.gov/ntp/roc/twelfth/Addendum.pdf November 7, 2011
- OSHA. Occupational Safety and Health Standards. Standard Number: 1910.1048 : Formaldehyde. United States Department of Labor, Occupational Safety and Health Administration, 2011; http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=10075&p_table=STANDARDS November 7, 2011
- Leica, Microsystems. Material Safety Data Sheet: 10% Millonig’s Buffered Formalin. 2007; http://www.leica-microsystems.com/index.php?id=1504&tx_leicaproducts_pi1[showUid]=3299&tx_leicaproducts_pi1[tab]=downloads&cHash=49baf1391ce5bcd25cd31e224782b369 27/10/2011
- Bozzola JJ, Russell LD. Electron microscopy: principles and techniques for biologists. Boston: Jones and Bartlett, 1992
Related Content
Leica Biosystems Knowledge Pathway content is subject to the Leica Biosystems website terms of use, available at: Legal Notice. The content, including webinars, training presentations and related materials is intended to provide general information regarding particular subjects of interest to health care professionals and is not intended to be, and should not be construed as, medical, regulatory or legal advice. The views and opinions expressed in any third-party content reflect the personal views and opinions of the speaker(s)/author(s) and do not necessarily represent or reflect the views or opinions of Leica Biosystems, its employees or agents. Any links contained in the content which provides access to third party resources or content is provided for convenience only.
For the use of any product, the applicable product documentation, including information guides, inserts and operation manuals should be consulted.
Copyright © 2025 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.



